From the beginning, 2020 was an extremely consequential year in a multitude of ways, but perhaps none more so than in health care. This traumatic and upheaval-filled year taught U.S. a great deal about the state of American health care, where its vulnerabilities are, where its strengths are, and where it might be going.
We Weren’t Ready
The biggest and most painful lesson was in the area of pandemic response. The U.S. has had years of warnings about preparedness for a new outbreak of a deadly disease. The year 2018 was filled with reminders of the one hundredth anniversary of the 1918 Spanish Flu and how we as a society need to get ready for the next one. In 2016, this author published “Shall We Wake the President: Two Centuries of Disaster Management from the Oval Office,’ (reviewed by inFOCUS Quarterly in summer 2017) which warned that “One specific area that could stand improvement is the development of coronavirus countermeasures.” In 2014, the U.S. had a brief Ebola scare in which we learned that our systems of infection controls were not as robust as they needed to be. And in the 2000s, President George W. Bush warned of – and took preliminary but crucial steps to protect from – a pandemic flu outbreak.
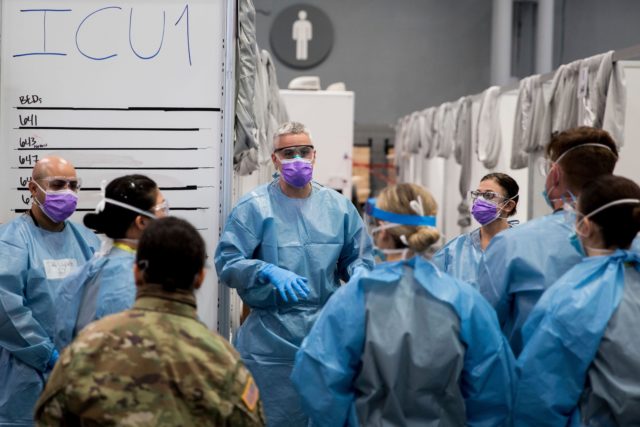
Despite all of these warnings, and despite billions of dollars spent in creating, filling, and maintaining the Strategic National Stockpile, when the SARS-Covid-2 outbreak occurred in 2020, the U.S. was not ready. We did not properly prepare for the disease before it came to our shores – to be fair, the Chinese government’s obfuscation helped here – we could not track and trace outbreaks via robust and effective testing once it got here, and we had no countermeasures in the form of vaccines or antivirals. When the biggest disease outbreak that the world had seen in a century came, all that the most advanced health care system in human history could do was… tell people to shelter in place and wash their hands. It was a humbling comedown for a society that was used to having technology fix its problems.
Politicizing the Health Care Community
The second disturbing lesson from 2020 was about the increasing politization of the public health community. The public health world, which is supposed to protect the public from the spread of deadly communicable diseases, had lost focus and started to exert more effort into the realm of non-communicable conditions created by human behavior. Instead of looking at pandemics, public health paid more and more attention to criticizing and trying to root out human behaviors like the consumption of large sodas. The focus became behavior modification rather than disease mitigation, and that may have contributed to the lack of preparedness for a once in a century pandemic.
Then, once the pandemic struck, the politicization continued, with disastrous effects. Initially, the public health community tried to downplay the risks, suggesting that flu shots and attending Chinese New Year celebrations were more important than worrying about a mysterious virus. Worse, as Americans started considering the adoption of face masks, something not natural in American culture, Surgeon General Jerome Adams tweeted: “Seriously people- STOP BUYING MASKS! They are NOT effective in preventing general public from catching #Coronavirus, but if healthcare providers can’t get them to care for sick patients, it puts them and our communities at risk!”
Later, it emerged that public health officials intentionally downplayed the use of masks, not because they were ineffective, but because they wanted to maintain supply levels for frontline health care workers. Making sure that supplies were adequate for the front line was and is an admirable goal, but the intentionally misleading communiques had a disastrous effect. Once public health officials discovered that masks did have some level of effectiveness at preventing the spread of a communicable airborne disease, changing the messaging encountered some skepticism among an American public long disinclined to mask wearing. The result was that masks unnecessarily became a political issue, and another flashpoint in the detrimental perceived war between conservatives and the public health community.
Conservatives, Social Protests and COVID-19
The tensions between the communities worsened over the summer during the Black Lives Matters protests. The public health community had been at the forefront of pushing for lockdowns and social distancing, and particularly critical of protests against those lockdowns. Yet when the BLM protests took place this summer, over 1,000 public health experts signed a letter giving their blessing to mass gatherings in the streets: “We created the letter in response to emerging narratives that seemed to malign demonstrations as risky for the public health because of COVID-19. Instead, we wanted to present a narrative that prioritizes opposition to racism as vital to the public health, including the epidemic response. We believe that the way forward is not to suppress protests in the name of public health but to respond to protesters demands in the name of public health, thereby addressing multiple public health crises.” To millions of Americans, the message seemed to be: all social activities are forbidden, except for ones that advance a preferred political agenda.
The disconnect between conservatives and the public health community was so stark that public health experts Lindsey Leininger and Harold Pollack wrote a piece in The Washington Post declaring that the public health community needed to do a better job communicating with conservatives. In the piece, Leininger and Pollack argued that public health needed to treat conservatives as another demographic group that required targeted outreach. They also pointed out that survey showed that 72 percent of public health officials considered themselves liberals, while only 4 percent classified themselves as conservatives. While this disconnect has existed and been widening for a while, 2020 showed that this disconnect had real world consequences in terms of the willingness of Americans to comply with public health pronouncements.
W’s Vaccine Strategy Success
On the positive side, one lesson we learned was that vaccine development had made incredible advances over a short period of time. When George W. Bush put together his pandemic preparedness plan, one of the plan’s long-term goals was to increase vaccine development capabilities. In fact, the Bush administration’s plan specifically called for a “crash program” to “accelerate cell culture technology.” For years, our egg-based vaccine development system had a host of vulnerabilities, including the limitations of the egg supply, susceptibility to allergic reaction in some, and imperfect levels of effectiveness in our annual flu vaccine.
Now, with the new flu vaccines, we are using even more advanced mRNA technology. The flu vaccines were developed in less than a year under the Operation Warp Speed initiative. This initiative called for active cooperation between the public and the private sectors, with the federal government standing as a guaranteed purchaser of the product, and the private sector being responsible for the development. This approach led to the development of two vaccines in record time, both with over 90% effectiveness, with other vaccine candidates emerging as well. The results from the vaccine in Israel, the world leader in vaccinations thus far, have been incredibly encouraging, with deaths, illnesses, and instances or transmission all going down. By all accounts, the development of the vaccine has been a stunning success.
Distribution Failures
Unfortunately, and at the same time, the distribution of the vaccine, particularly in the U.S., has been a disappointment. The reason that the paragraph above refers to the impressive results in Israel is that the distribution there has been sufficiently efficient and widespread to enable us to see these impressive results. In the U.S., though, distribution has not been nearly as efficient, and the very success of the vaccine development has been diminished by the confusion and disorganization of its distribution. Instead of focusing solely on getting vaccines to the highest risk people, or to the greatest number of people in the shortest amount of time, CDC and state public health officials allowed political considerations to affect the prioritization of vaccines. This was yet another instance in which the politicization of public health got in the way of responding to the coronavirus. In addition, distribution challenges beyond the politicized prioritization process meant that the demand for shots far exceeded the available supply of them in the crucial early months of the vaccine when the U.S was trying to stem the tide of the virus.
Given these lessons, the question going forward should be how we can take the lessons of 2020 – and some of 2021 – and apply them to making sure that something like this never happens again. The overwhelming costs of the virus in the U.S., hundreds of thousands of dead, trillions of dollars spent, U.S. credibility severely damaged, and national vulnerabilities exposed for enemy state and non-state actors alike. If there is to be another deadly pathogenic outbreak in the future, the U.S. will have to have a far better response than what we witnessed in 2020.
Lessons for the Future
To do better in the future will require a careful examination of this recent past and a willingness to do better next time. The first lesson and required improvement is in the area of international monitoring. We will of course need to be more skeptical of information coming from China next time, but there is no guarantee that the next outbreak will come from China. In the future, the U.S. will have to be both more active and skeptical of official reports when it comes to international monitoring. Since the U.S. can’t be everywhere, this will entail international cooperation and working with the World Health Organization (WHO). Unfortunately, the WHO’s continued unwillingness to hold China to account suggests that the U.S. and its allies have a lot of work to do in terms of trying to reform the WHO to make it a better partner in the future.
The second area of required improvement is in the area of domestic monitoring and testing. Clearly, reliance on CDC to develop the testing needed to measure an outbreak in the future will not work. Going forward, the U.S. will have to learn the lessons from Operation Warp Speed and ensure that there is active cooperation between the private and public sector, allowing the public sector to set direction and indicate governmental needs, but to allow the private sector to do what it does best in terms of developing and manufacturing the required tests.
Third, the U.S. must rethink its Strategic National Stockpile (SNS) in the future and ensure that it focuses on more nimble platforms and less on specific hit or miss products. The groundbreaking mRNA success of Operation Warp Speed indicates that the U.S. does not need to have vaccine on hand for a particular pathogen so much as the ability to develop a vaccine – quickly – for whatever pathogen comes our way.
Finally, the key lesson of 2020 is the need to depoliticize public health. Public health should focus on the hard science of preventing and or mitigating the spread of deadly diseases rather than the soft non-science of advancing its political preferences. Focusing on politics rather than disease prevention leaves officials unfocused on the deadliest problems we face, weakens our ability to respond, and perhaps worst of all, damages the credibility of public health among large sections of the population at the very moments when we most need population-wide adherence to science-based disease prevention guidelines. We cannot know what pathogens we may face in the future, but we already do know what we need to do now to prepare for what may come.
Tevi Troy, Ph.D., is a presidential historian, a former White House aide, and a JPC Fellow. His latest book is “Fight House: Rivalries in the White House from Truman to Trump.”





